Is There Really Such Thing As Leaky Gut?
Is There Really Such Thing As Leaky Gut?
Sometime during 2015 I was told I had “leaky gut.” I had no idea what it meant or if it was an actual diagnosis. I had not heard the term in college or any of my time working at Johns Hopkins Hospital. In December 2016, I was accepted and attended the 3-day preceptorship program at the University of Chicago Celiac Disease Center. During a presentation, one of the gastroenterologists talked specifically about “leaky gut” or what is called intestinal permeability. Now, more doctors are seeing leaky gut as an issue. Dr. Alessio Fasano, a gastroenterologist and a world-renowned expert on intestinal permeability is doing much research on this topic.
What is intestinal permeability (leaky gut)?
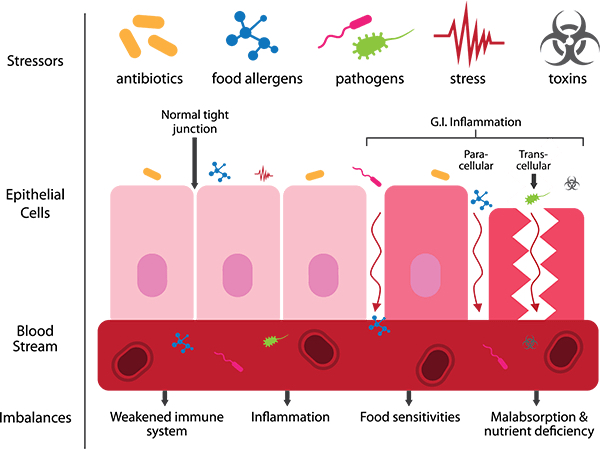
The intestine is lined with a layer of cells. There are small gaps in the intestinal wall (tight junctions) that allow small molecules (such as water, electrolytes and other nutrients) into the bloodstream to be used by the body. This layer also helps keep harmful substances out of our bloodstream. In someone with “leaky gut” these tight junctions are not working properly. When these gaps become loose, food may not properly break down before they slip through. The gut is now more permeable. This can also allow bacteria and toxins to enter the bloodstream. The body looks at these as invaders and starts an immune and inflammatory response.
Symptoms
When harmful substances get through the intestinal lining into the bloodstream symptoms can include bloating, digestive issues, fatigue, muscle aches and pains, confusion, and skin issues. These invaders tend to target different areas in the body, making symptoms vary from one individual to another.
Link with autoimmune disease
It is thought that leaky gut is a precursor to autoimmune disease. The immune system reacts when the proteins, bacteria, and viruses slip through the junctions. This in turn can trigger an immune response in those that are genetically susceptible. Multiple diseases can arise or be exacerbated due to leaky gut, including Crohn’s disease, celiac disease, Type 1 diabetes, multiple sclerosis, irritable bowel syndrome (IBS), asthma, cancer, food allergies and intolerances, and rheumatoid arthritis.
What contributes to intestinal permeability?
A variety of internal and external irritants can contribute to leaky gut, such as chemicals in processed foods, alcohol, pollutants, radiation & chemotherapy, NSAID use (such as indomethacin, ibuprofen and naproxen), trauma and burns, and viral or parasitic infections.
Testing for leaky gut
The only test used to monitor intestinal permeability is the lactulose-mannitol challenge. This is used mostly in research, but available in some commercial labs.
Dr. Fasano and his colleagues have focused much of their research on zonulin, which is a human protein. Zonulin tends to widen the intestinal cell junctions, which is thought to cause leaky gut. Based on research, people with an autoimmune disease tend to release more zonulin than the average population, making them more prone to leaky gut. Bad gut bacteria and gluten (via gliadin) are two of the most powerful triggers of zonulin release.
Can leaky gut be treated?
This is an area with a large variety of opinions, but some points that are agreed on are:
Removing gluten from the diet. Make sure to get a celiac antibody test prior to going gluten-free to rule out celiac disease.
Monitor for food allergies or any food intolerance. Based on this, treat with the appropriate diet.
Correct nutritional deficiencies.
*Restore healthy bacteria in the gut with a probiotic.
Other suggestions for helping to treat leaky gut:
Encourage whole-foods, anti-inflammatory diet. This could be the Mediterranean or Paleo diet. The Paleo diet appears to be a more popular choice amongst those with leaky gut and those treating leaky gut.
Decrease alcohol intake if consuming.
Decrease intake of NSAIDs.
*L-glutamine (an amino acid)- Thought to help with growth and repair of intestinal lining.
*Zinc (essential trace element)- Thought to help resolve permeability changes.
*Saccharomyces boulardii (nonpathogenic yeast-a probiotic)
*Prior to starting any supplement or vitamin get your physician’s approval first.
Future treatments
Larazotide acetate is being studied to help those with celiac disease that follow a gluten-free diet, but continue to have symptoms. This drug is a tight junction regulator, which can help restore the open junctions (“leaky gut”). In celiac disease, exposure to gluten causes these junctions to open, thus leading to an inflammatory reaction. This medication is also being looked at for others that have intestinal permeability for a variety of other reasons. This medication is still currently being studied.
References:
Stewart E.A. CPE Monthly: Leaky Gut Syndrome-Learn About the Causes, Associated Conditions, and Treatments Under Research. Today’s Dietitian. January 2016. Vol. 18 No. 1 P. 46.
Fasano A. Episode 32: Leaky Gut with Dr. Alessio Fassano. PheonixHelix.com
The information in this blog is not a substitute for professional medical advice, examination, diagnosis and treatment. Always seek the advice of your physician or other qualified healthcare provider before altering your diet, starting a new treatment or making changes to an existing treatment.
Meet Valerie
Registered Dietitian Nutritionist - CDN, RDN
My name is Valerie Polley. I am a Indianapolis-based registered dietitian and owner of Blue Tree Nutrition. I consult with clients both local and far away.
I have a bachelor’s degree in nutrition from Purdue University and I have been practicing for 20 years.
I thoroughly enjoy helping clients through their gut health journey. I see a range of GI issues including, but not limited to celiac disease, IBS and SIBO. I also specialize in the FODMAP elimination diet.
Subscribe for More Great Articles!
Subscribe via email to be notified of new articles, healthy recipes and helpful tips.


Recent Comments